What is Pediatric Sleep Apnea?
Sleep Apnea is a sleep disorder in which breathing continuously starts and stops throughout the night[1]. This decreases the blood oxygen levels, causing the sleeper to wake up suddenly to breathe normally again and raise the blood oxygen levels1. Usually sleep apnea episodes last about 10 seconds or more and occur repeatedly through the night, but as mentioned, sleepers are often unaware that this is happening[1].
There are two main types of sleep apnea: obstructive sleep apnea (OSA) and central sleep apnea (CSA)[1].
OSA is caused by an obstruction in the back of the throat when the soft tissue in the back of the throat relaxes, and blocks the airway[1]. CSA, on the other hand, is a central nervous system issue, caused by the brain’s inability to interpret signals to breathe[1].
Most people – including children – who have sleep apnea, have obstructive sleep apnea.
The main difference between OSA in children and adults is that pediatric OSA is most commonly due to enlarged tonsils and adenoids while the condition is likely (but not always) associated with obesity in adults[2]. Children are also more likely to exhibit behavioral side effects, whereas adults usually complain of daytime sleepiness[2].
Can Toddlers Have Sleep Apnea?
According to Yale Medicine, about 2 to 3 percent[3] of children are believed to have sleep apnea, and the disorder may be present in up to 10 to 20 percent of children who habitually snore.
Apnea symptoms tend to occur more frequently in premature infants and newborn babies, compared to older children[2]. Sleep apnea is also more common in children born with certain conditions like Down syndrome, cerebral palsy, sickle cell disease, low birth weight, or birth defects of the skull or face[2]. The reason behind the sleep apnea will likely determine the type of sleep apnea the child has.
- Central sleep apnea happens when the brain fails to send proper signals to the muscles that regulate breathing. This condition is more common[4] in premature infants whose central nervous system has yet to develop, as well as children who have experienced brain injuries or who have brain masses.
- Obstructive sleep apnea usually happens in children due to a narrowing of the upper airways when they are lying down to sleep. In children, this is most commonly caused by unusually large adenoids or tonsils[2].
- Mixed apnea[5] refers to a condition in which an obstructive apnea immediately follows a central apnea. This is the most common type of apnea in premature infants[6].
Most apneas in babies are due to an immature brainstem[7] or secondary medical conditions, like Down syndrome, cerebral palsy, or certain birth defects[2]. When pauses in breathing are due to developmental delays, most infants will outgrow this by the time they are one year old[8].
For children older than one, though, research shows us there are two main “peak periods[9]” that show signs of OSA. The first is during preschool age, when tonsils or adenoids will be the most likely culprit[9]. The second peak period happens during adolescence, when obesity is the most likely contributing factor[9].
Pediatric Sleep Apnea Symptoms to Watch For
Many of the symptoms of OSA appear in the first few years of life but most cases are not diagnosed until many years later. OSA in early childhood can slow growth, but following sleep apnea treatment, most children show advancements in both height and weight[2]. While every child is different, we’ll highlight some of the most common symptoms of pediatric sleep apnea.

Snoring
Noisy breathing or loud snoring during sleep may be a symptom of apnea2. However, snoring can also occur in healthy children. If you are concerned about your child’s snoring, we suggest consulting your pediatrician.
If your child snores at night, a good mattress for snoring could help.
Bedwetting
Bedwetting is another symptom that can be very common in children without sleep apnea, but can also occur due to apneic episodes[2]. Again, if you’re worried about your child’s bed wetting, it is wise to consult a medical professional.
Night Terrors
Night terror episodes[10] involve screaming, flailing, and intense fear that occurs while children are still asleep. Sleep apnea can be an underlying cause of night terrors in children[10].
Teeth Grinding
Grinding or clenching the teeth[11] at night is referred to as bruxism and can lead to sore jaw muscles, sensitive teeth, and increased tooth decay. People with sleep apnea are more likely to grind their teeth[11].
Frequent Infections
Chronic ear infections, tonsillitis, strep throat, and swollen adenoids may all occur more frequently in children with sleep apnea compared to other children[9].
Disordered Breathing
Periods of normal breathing with subsequent pauses or breath-holding is one of the most common signs of sleep apnea, so look out for this if your child is exhibiting other sleep apnea symptoms[2].
Restlessness
Children with sleep apnea may toss and turn all night long, rarely entering a deep state of sleep[2]. This side effect of sleep apnea can lead to excessive daytime sleepiness.
Mouth Breathing
If air entry through the nose is blocked due to enlarged tonsils or adenoids, children with sleep apnea may mostly breathe through the mouth instead of their nose[2].
Odd Sleep Positions
Sleeping in abnormal positions[12] could be a sign the child is trying to open their airways for easier breathing. Some abnormal sleeping positions may include sleeping with the neck arched backward, sleeping in a seated position, or sleeping with an arched back.
Signs of Pediatric Sleep Apnea During the Daytime
Adults with sleep apnea are more prone to drowsiness during the daytime because of fragmented sleep[1]. Every time they have pauses in breathing, they wake up briefly, preventing them from getting a good night’s rest[1].
Children, on the other hand, have a higher “arousal threshold[13]” than adults, so children with sleep apnea wake up less frequently. Research[14] indicates that children’s daytime symptoms could be due to poor sleep, as well as hypoxia, which indicates low blood oxygen levels during the night. We’ll explain some of the signs you can look out for in a child with sleep apnea.
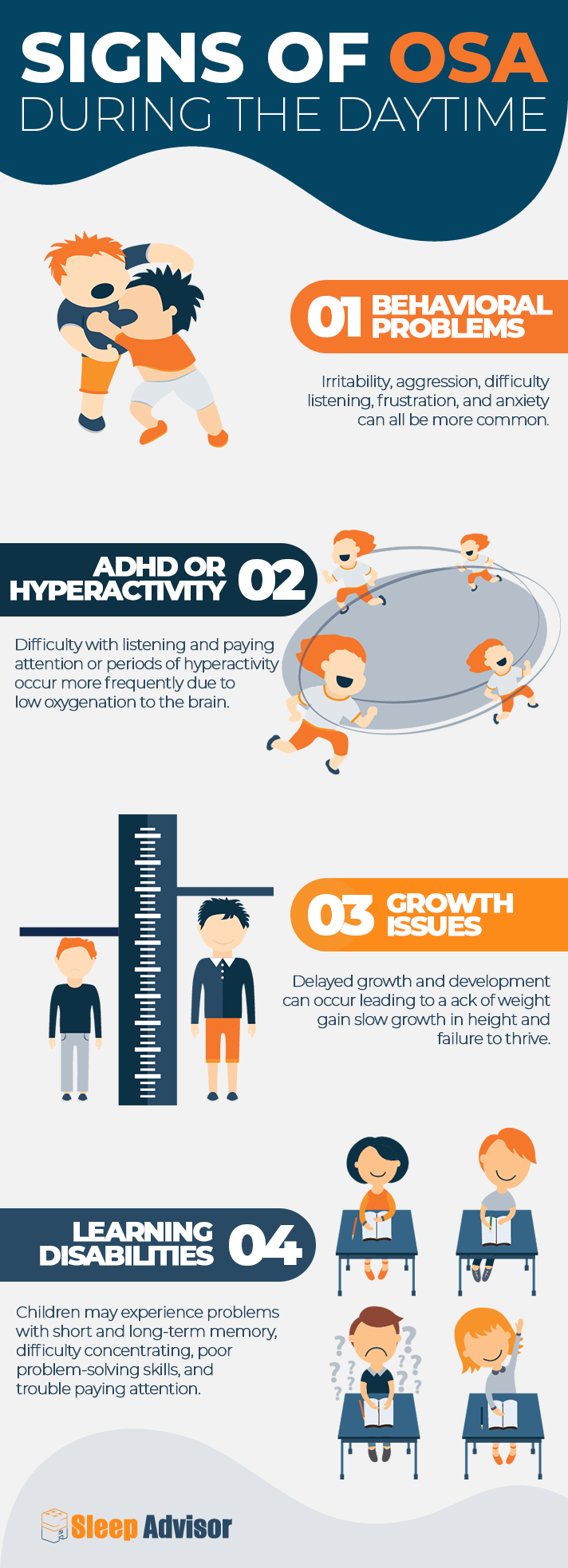
Behavioral Problems
Irritability, aggression, difficulty listening, frustration, and anxiety can all be more common in children with sleep apnea, due to a lack of sleep and low blood oxygen levels[14].
ADHD or Hyperactivity
Difficulty listening and paying attention, or periods of hyperactivity occur more frequently in children with sleep apnea due to low oxygenation to the brain[14].
Growth Issues
Delayed growth and development can occur for those who experience pediatric sleep apnea, leading to a lack of weight gain, slow growth in height, and a slower rate of cognitive development[2].
Learning Disabilities
Children with sleep apnea may experience problems with short and long-term memory, difficulty concentrating, poor problem-solving skills, and trouble paying attention due to their poor sleep quality and hypoxia[2].
How Dangerous is Pediatric Sleep Apnea?
It is important to speak to your child’s doctor if you are concerned about their breathing. If their physician believes there is a reason to suspect sleep apnea, they will likely refer your child to a specialist such as an ear, nose, and throat doctor (ENT) or pulmonary (lung) specialist for further investigation.
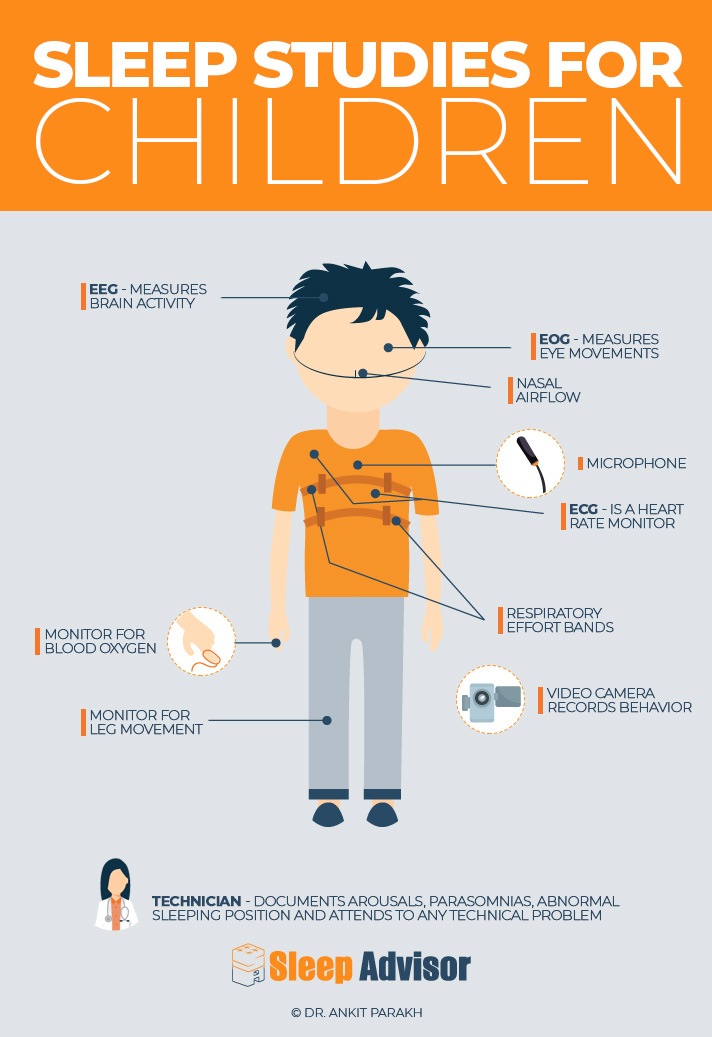
Testing[15], including evaluation of the upper airways, X-ray, and overnight sleep studies, may be used to determine the presence and extent of sleep apnea in your child. When your doctor meets with you to discuss the results, they will generally let you know how severe your child’s apnea is and what treatment is recommended.
Sleep apnea can have some serious complications, including high blood pressure, poor growth, and heart problems[2]. This condition can also impact learning and behavior, so it is important to have it diagnosed and treated early[14].
In severe cases of sleep apnea that are left untreated, there is a risk of death, albeit small. According to one study[16] looking at morbidity and mortality in 2,998 children ages 0-19 with a diagnosis of OSA, the 5-year mortality rate was 0.7 percent. While this percentage is small, there is still a risk of death associated with severe pediatric sleep apnea.
What Causes Pediatric Sleep Apnea?
Many factors play a role in the development of sleep apnea. For premature and newborn babies, the development of this condition is often due to an immature central nervous system and/or respiratory system[6]. Other risk factors of sleep apnea include certain developmental disabilities, musculoskeletal abnormalities, and body weight[2].
Obesity
In older children (around the age of adolescence) OSA may occur more often due to obesity. According to research[17], obese children who develop sleep apnea experience changes to their respiratory systems from increased tissue mass putting pressure on their neck and lungs, narrowing the airways and inhibiting normal breathing.
Learn More: Obesity and Sleep
Neuromuscular Disease
Children with neuromuscular diseases are at a higher risk of developing OSA due to the weakening of muscles in the upper airway[2]. This weakness contributes to increased resistance at night because these muscles are required to maintain an open airway[2].
Cerebral Palsy
Neurodevelopmental disabilities such as cerebral palsy can also increase the risk of OSA because of low muscle tone and various other malformations in the upper airway[2].
Abnormalities in Skull or Muscles
Many deformities in the cranial or musculoskeletal system can result in nasal or nasopharyngeal obstruction, blocking off the airway[2]. Low or poor muscle tone also prevents full inhalation and exhalation, increasing the likelihood of apnea[2].
Sickle Cell Disease
Sickle cell disease[18] is a condition characterized by chronic hemolytic anemia, or the abnormal breakdown of red blood cells. There is an increased prevalence of OSA in kids with sickle cell disease, although the exact rate is uncertain with a wide variation between 5 to 79 percent in various studies[19].
Questions for Your Doctor
What treatments are available?
Treatments for pediatric sleep apnea can vary based on the underlying cause. While some children may outgrow this condition, others will require treatment that may involve surgery to remove the tonsils and adenoids, correction of craniofacial abnormalities, weight loss interventions, or continuous positive airway pressure (CPAP) devices[2].
Will my child need surgery?
Enlarged tonsils and adenoids are the most common causes of OSA in children, resulting in frequent infections and difficulty breathing[2]. Surgical removal of the tonsils (tonsillectomy) and adenoids (adenoidectomy) is often recommended in this case. Sometimes, surgery to fix craniofacial malformations is also necessary.
Can my child use CPAP therapy?
If surgery is not effective or recommended, using a CPAP machine may be an option for your child. CPAP Therapy[20] involves wearing a mask over the mouth or nose that holds the airway open by gently blowing in the air at a continuous pressure. The mask is generally worn overnight and during any naps as well[20].
Learn More: Best CPAP Masks for Kids
Is there another oral appliance that may work better than a CPAP device?
Oral devices are an alternative to traditional CPAP masks and work by pushing the tongue and jaw forward, making the airway larger and increasing airflow. Some studies[21] have found that oral appliances are better tolerated in children than CPAP machines because they are quieter, more comfortable, and more portable.
Natural Treatments for Pediatric Sleep Apnea
Like many other conditions, there are some natural treatments and home remedies for sleep apnea that may be worth exploring. Remember that this condition can be very serious, and it is always important to speak with your child’s doctor before using any natural treatments.
More Exercise
Regular exercise is important for improving the cardiovascular system, increasing energy, and maintaining a healthy weight[22]. Yoga may be a great choice because it can strengthen the respiratory system[23] and improve oxygen flow.
Better Diet
Changing your child’s diet to include more anti-inflammatory foods[24] like fruits and vegetables can be a great way to support the body and respiratory system. A healthy diet is also important in cases where body weight may be contributing to OSA.
Use a Humidifier
Humidifiers are used to help moisten the air, preventing dryness in the airways. Many CPAP devices have built-in humidification, but humidifiers can also be useful even when CPAP devices aren’t recommended. Certain essential oils such as lavender, marjoram, and thyme can also be added to some humidifiers and/or CPAP devices to help reduce inflammation and improve apnea.
Remove Allergens and Pollutants
Many allergens like dust, cigarette smoke, and pet hair can make sleep apnea symptoms worse[25]. Allergens and pollutants can increase inflammation, narrowing the airways and making breathing more difficult. Opening the windows, vacuuming frequently, and using an air filtration system can also be helpful.
If your child has issues with allergies, take a look at our list of best mattresses for allergy and asthma.
Change Position or Use Wedge Pillow
Sleeping in a supine position (on the back) often makes sleep apnea symptoms worse[26]. You can try to get your child to sleep on their side, but oftentimes, if somebody is used to sleeping on their back, they’ll find their way back to their favorite position. In this case, try using a wedge pillow. Studies have shown that elevating the head[27] in this way can improve sleep apnea symptoms.
Conclusion
Sleep apnea is a serious condition that can occur in children of all ages, shapes, and sizes. If you are worried that your child may be displaying some of the signs and symptoms, including snoring, restlessness, or worsening behavior, it is important to speak with their doctor for evaluation and a proper diagnosis.
With treatment, most children can recover from sleep apnea or better manage their symptoms long-term.

Raina Cordell
RN, RHN, Certified Health Coach
About Author
Raina Cordell is a Registered Nurse, Registered Holistic Nutritionist, and Certified Health Coach, but her true passion in life is helping others live well through her website, www.holfamily.com. Her holistic approach focuses on the whole person, honing the physical body and spiritual and emotional well-being.
Combination Sleeper
- “Sleep Apnea”. National Institute of Neurological Disorders and Stroke. Last modified January 20, 2024.
- “Pediatric obstructive sleep apnea”. Mayo Clinic. Last modified February 21, 2024.
- “Pediatric Obstructive Sleep Apnea”. Yale Medicine. Webpage accessed July 2, 2024.
- “Central Sleep Apnea (CSA) in Children”. Children’s Hospital Colorado. Webpage accessed July 1, 2024.
- Herkenrath, Simon., Pavsic, Katja., et. al. “Mixed apnea metrics during diagnostic polysomnographies in obstructive sleep apnea patients with/without treatment-emergent central sleep apnea”. European Respiratory Journal. 2019.
- Kondamudi, Noah P., Krata, Lewis., Wilt, Andrew S. “Infant Apnea”. National Library of Medicine. 2024.
- “Apnea in Infants”. Nicklaus Children’s Hospital. Last modified January 28, 2021.
- “Apnea”. Nationwide Children’s. Last modified July 2022.
- Nino, Gustavo., Restrepo-Gualteros, Sonia M., Gutierrez, Maria J. “Pediatric sleep apnea and viral respiratory infections: what do clinicians need to know?” National Library of Medicine. 2022.
- “Sleep terrors (night terrors)”. Mayo Clinic. Last modified April 23, 2021.
- “Bruxism (teeth grinding)”. Mayo Clinic. Last modified August 10, 2017.
- Sockrider, Marianna., Rosen, Carol L., Farber, Harold J. “Obstructive Sleep Apnea In Children”. American Thoracic Society. 2021.
- Marcus, Carole L. “Arousal Threshold in Obstructive Sleep Apnea”. ATS Journals. 2014.
- Csábi, Eszter., Gaál, Veronika., et. al. “Increased behavioral problems in children with sleep-disordered breathing”. BMC. 2022.
- “Pediatric Sleep Study”. Yale Medicine. Webpage accessed July 1, 2024.
- Jennum, Poul., Ibsen, Rikke., Kjellberg, Jakob. “Morbidity and mortality in children with obstructive sleep apnoea: a controlled national study”. National Library of Medicine. Thorax. 2013.
- Bhatt, Surya Prakash., Guleria, Randeep., Kabra, S. K. “Metabolic alterations and systemic inflammation in overweight/obese children with obstructive sleep apnea”. Plos One. 2021.
- “What Is Sickle Cell Disease?”. National Heart, Lung, and Blood Institute. Last modified July 22, 2022. .
- Rosen, Carol L., Debaun, Michael R., Strunk, Robert C., et. al. “Obstructive sleep apnea and sickle cell anemia”. National Library of Medicine. 2014.
- “CPAP”. National Heart, Lung, and Blood Institute. Last modified March 24, 2022.
- Idris, Ghassan., Galland, Barbara., et. al. “Efficacy of a Mandibular Advancement Appliance on Sleep Disordered Breathing in Children: A Study Protocol of a Crossover Randomized Controlled Trial”. National Library of Medicine. 2016.
- “7 Heart Benefits of Exercise”. Johns Hopkins Medicine. Webpage accessed July 1, 2024.
- Yamamoto-Morimoto, Kuniko., Horibe, Shuji., et. al. “Positive Effects of Yoga on Physical and Respiratory Functions in Healthy Inactive Middle-Aged People”. National Library of Medicine. 2019.
- “Foods that fight inflammation”. Harvard Health Publishing. 2021.
- Chirakalwasan, Naricha., Ruxrungtham, Kiat. “The linkage of allergic rhinitis and obstructive sleep apnea”. National Library of Medicine. 2014.
- Omobomi, Olabimpe., Quan, Stuart F. “Positional therapy in the management of positional obstructive sleep apnea-a review of the current literature”. National Library of Medicine. 2018.
- Souza, Fábio José FB., Genta, Pedro Rodrigues., et. al. “The influence of head-of-bed elevation in patients with obstructive sleep apnea”. National Library of Medicine. 2017.
