One minute everyone is singing the praises of a low-fat diet, the next minute fats are good again but carbs are bad. What gives? Trying to be healthy can be so confusing!
And who has time for it all anyway? Work out 30 minutes a day, make all your food from scratch, and somehow still manage all your stress. Your idea of stress-relief is a glass of wine – okay, maybe the whole bottle (don’t worry I won’t tell).
Now your doctor is asking if you’re getting enough sleep? Is he crazy? Who has time for sleep! In the 21st century, if you snooze… you lose, right? Well, maybe not. Getting enough shut-eye may be more important than you think, especially when it comes to your heart.
Doctors have been preaching about the health pillars of diet and exercise for years, but it turns out they’ve been missing one. Research on the subject of sleep and heart health is growing, and there are plenty of studies that show too little or too much sleep can place a serious strain on your heart.
How exactly does sleeping impact the cardiovascular system, and is there a sweet spot when it comes to sleep? Keep reading for everything you need to know about sleep and your heart, including how to improve cardiovascular health with better rest.
What is Cardiovascular Disease?
To start with, let’s look at the heart and how it works. The heart is the primary organ of the circulatory system, pumping blood that carries oxygen and nutrients to the tissues throughout the body while removing carbon dioxide and other waste products. According to Dr. Lawrence Phillips, an NYU cardiologist, the physiology of the heart comes down to “structure, electricity and plumbing”. [1]
The heart pumps blood through two systems known as the systemic circuit and the pulmonary circuit. The pulmonary circuit pumps blood through the lungs to gather oxygen. The systemic circuit supplies the heart and the rest of the body with oxygenated blood.
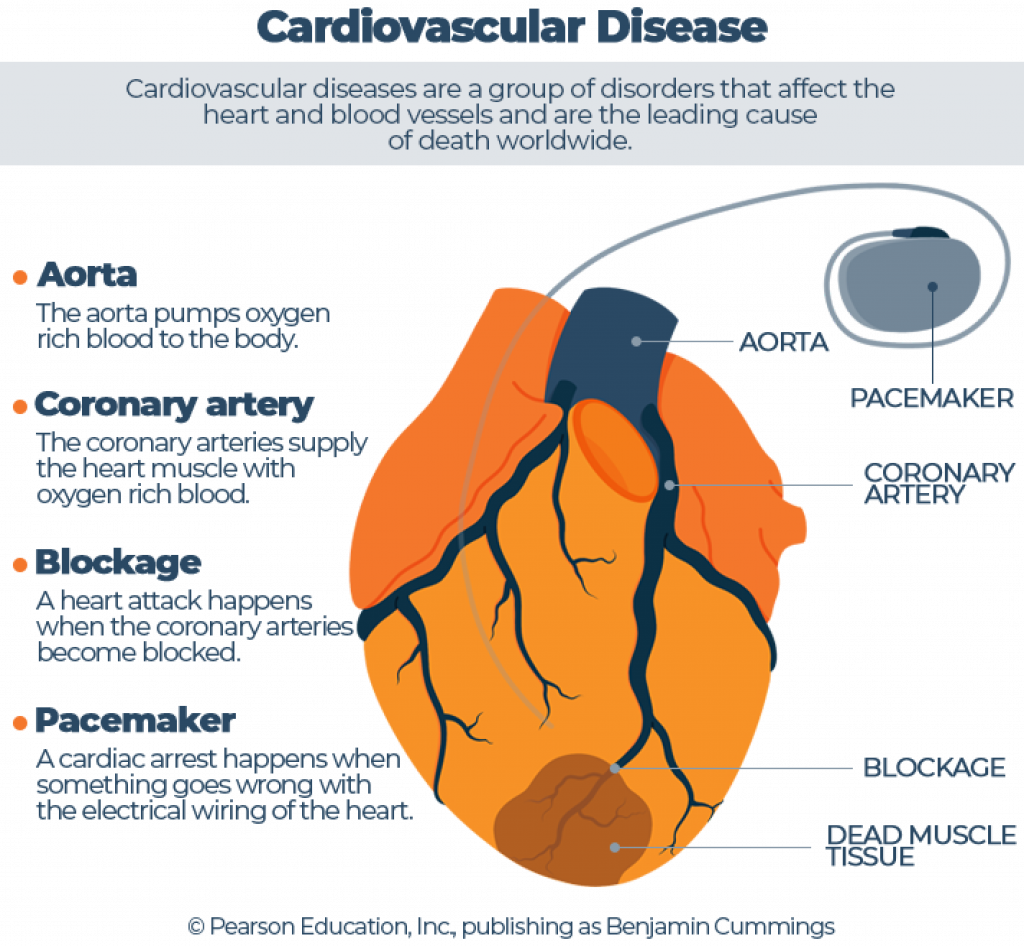
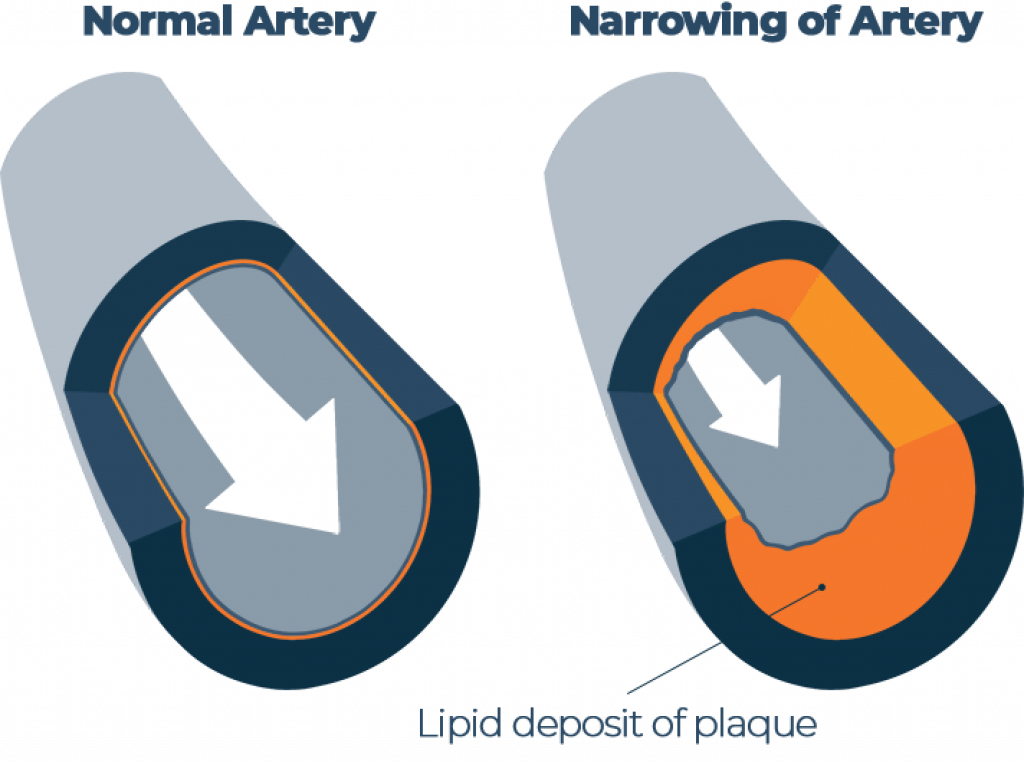
Like every other muscle in the body, the heart requires a constant supply of oxygen and other nutrients to be able to function, supplied through the coronary arteries. Kind of like the pipes in your home, these arteries can become damaged or clogged over time. If these passages become too narrow and cut off the supply of oxygen, the dangerous and often fatal consequence is a heart attack.
A cardiac arrest usually happens when something goes wrong with the electrical wiring, known as the pacemaker. Sometimes the vessels that supply oxygen to parts of the body also become blocked. When a blockage occurs in the brain, it’s known as a stroke.
How Common is Heart Disease?
Most people worry about dying from cancer or in a car accident, but cardiovascular disease (CVD) is the leading cause of death for both men and women worldwide. [2]
The WHO classifies cardiovascular diseases (CVDs) as:
- “coronary heart disease – disease of the blood vessels supplying the heart muscle;
- cerebrovascular disease – disease of the blood vessels supplying the brain;
- peripheral arterial disease – disease of blood vessels supplying the arms and legs;
- rheumatic heart disease – damage to the heart muscle and heart valves from rheumatic fever, caused by streptococcal bacteria;
- congenital heart disease – malformations of heart structure existing at birth;
- deep vein thrombosis and pulmonary embolism – blood clots in the leg veins, which can dislodge and move to the heart and lungs.”
Currently, 28.2 million Americans have a diagnosis of heart disease, and coronary heart disease is the most common. Alarmingly, 735,000 people will suffer a heart attack this year in the United States, many of whom have never even received a diagnosis of CVD before. That could be you, me, or the neighbor you’ve been waving to every morning for the past 10 years.
Some of the biggest risks for CVD are lifestyle factors like excess weight, inactivity, and stress – things that are all too common in the lives of Americans living in the 21st century. But the United States isn’t the only country with this issue. Worldwide, nearly 18 million people died from cardiovascular disease in the year 2016, with over 85% of these deaths due to heart attack and stroke. [3]
As I’m sure you’ve noticed, health is trending. Many of us are taking these overwhelming statistics to heart (quite literally) and are looking at ways to lower our risks. While smoking cessation, weight loss, and exercise programs can help, one of the most overlooked elements that has a direct impact on the heart, is sleep.
Effect of Sleep Deprivation on the Circulatory System
You’ve likely seen some funny memes about “your brain on too little sleep.” Without rest, your brain can’t function properly and you suffer the effects in areas like memory recall, learning, response times, and mental health. Knowing that one of the functions of the heart is to supply the brain with oxygen, it may be even more important to consider the effects of sleep deprivation on the organ that is central to supporting life throughout the body.
Similar to the brain, the effects of sleep deprivation on the heart are widespread. Consider your average middle-aged adult (Let’s call him Tom) who works long hours at a stressful job, only to come home and face additional demands trying to balance life with his wife and kids. Most nights, he goes to bed around midnight, often struggling to fall and stay asleep, only to wake up at 5 am and start the whole process over.
While sleeping, many organs in the body go into a resting state, a crucial time of healing and repair. This “downtime” is signaled by the brain in response to hormones and other chemical messengers known as neurotransmitters.
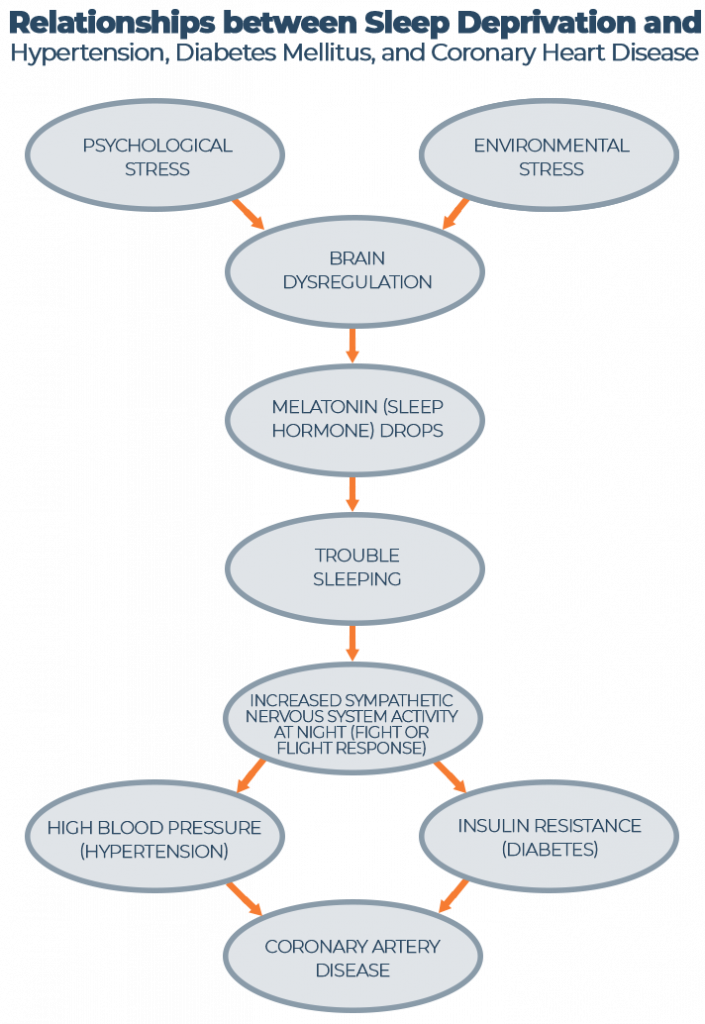
Normally, heart rate and blood pressure drop at night, remaining steady during NREM sleep and being similar to waking hours during REM stages. Sleeping too little places the body in a fight-or-flight state thanks to overstimulation of the sympathetic nervous system. Like a gas pedal that is continually floored, this perpetual overdrive can flood the body’s engine, burning out its circuitry.
Back to our friend and what happens to his heart when he loses out on even just a couple of hours of shut-eye each night. First of all, Tom’s heart rate increases and remains that way because he isn’t getting much of the deeper NREM stages of rest. This increased pumping places strain on the heart, building up pressure in the vessels, a condition known as hypertension.
Over time, high blood pressure coupled with high cholesterol (and several other factors which we will discuss next) can lead to hardening of the coronary arteries, or atherosclerosis. For Tom, sleeping just 5-6 hours per night means that he is much more likely to suffer from calcification of his arteries over the next several years than if he were getting at least 7-8 hours. [4]
Tom’s sympathetic nervous system also triggers the release of the hormone, cortisol. This stress hormone increases blood pressure and plays a role in energy metabolism, signaling the release of glucose and increasing blood sugar. As Tom continues to skimp on shut-eye, levels of hunger/satiety hormones, leptin and ghrelin, begin to fluctuate, leading to weight gain.
Poor Tom is feeling awful all the time and finally decides to go see his doctor. His blood work reveals increased CRP (an inflammatory marker), elevated thyroid hormone levels, and levels of blood glucose that warrant a diagnosis of type 2 diabetes. Tom is also diagnosed with hypertension and referred to a cardiologist who later confirms coronary artery disease. YIKES!
Too Much Shuteye is Equally Risky
While the harmful effects of sleep deficiency frequently make their way into mainstream news, nobody really talks about what happens when you go beyond the recommended 7-8 hours of shut-eye. It turns out, sleeping too much may be just as detrimental when it comes to heart health. A review of 15 studies spanning 25 years of research found that sleeping 9 or more hours per night increased the risk of developing or dying from coronary heart disease by 38% and the risk of stroke by 65%.
Just like when we don’t get enough rest, making a habit of sleeping in every day has been linked to increased inflammation, diabetes, obesity, heart disease, and stroke. Kind of like with vitamins and food, more of a good thing isn’t necessarily better.
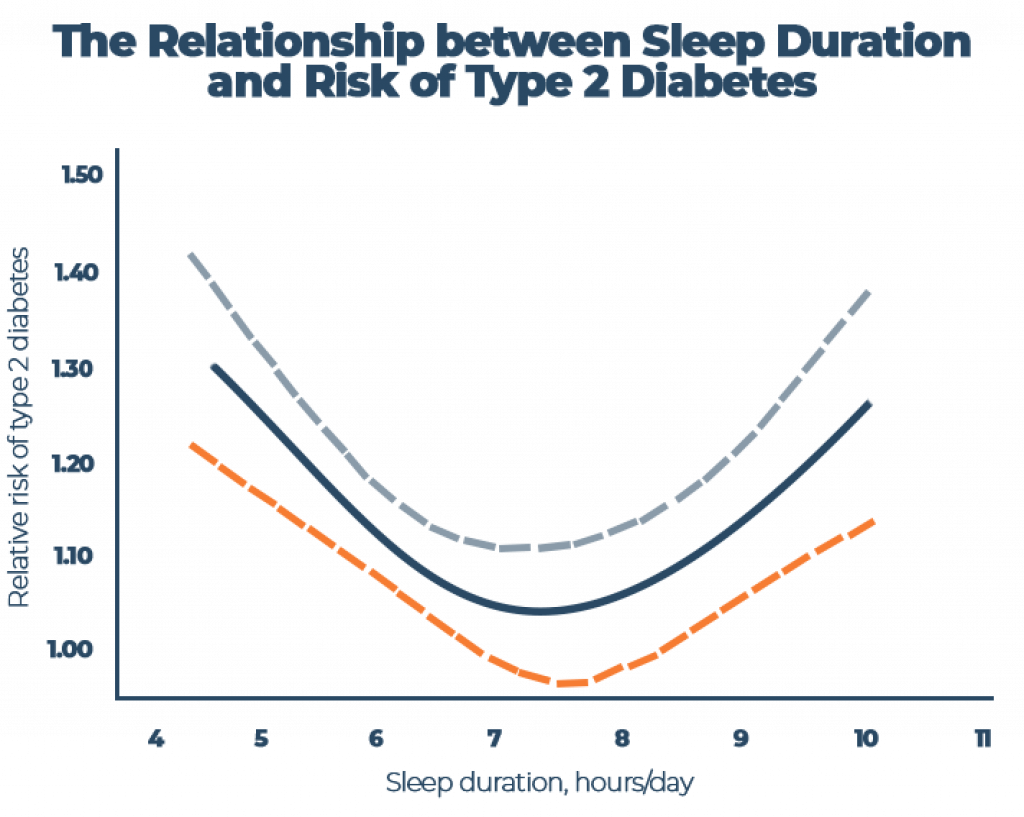
Is there a sweet spot when it comes to sleep? According to some research, there may be! Plenty of studies have found that 7 hours of slumber is associated with the lowest morbidity and mortality rates, as well as longevity and better brain health. However, the optimal amount will vary from person to person based on things like age, ethnicity, and genetics.
Links to Heart Disease: What Studies Show
Over the last 50 years, the average night of sleep has shortened by 1.5-2 hours per person. Not surprisingly, as the hours of shut-eye have decreased, the prevalence of all types of cardiovascular disease has increased. Lack of sleep triggers a stress response, decreasing melatonin secretion (our sleep-inducing hormone) and stimulating the sympathetic nervous system, which can lead to a number of serious consequences like high blood pressure and insulin resistance.
A recent study published in the Journal of the American Heart Association followed more than 1,600 adults with high blood pressure, Type 2 diabetes, heart disease, or stroke over a 20-year period to determine if sleeping less than 6 hours per day was associated with an increased risk of death. Their findings were staggering.
The researchers found:
- “Of the 512 people who passed away, one-third died of heart disease or stroke and one-fourth died due to cancer.
- People who had high blood pressure or diabetes and slept less than 6 hours had twice the increased risk of dying from heart disease or stroke.
- People who had heart disease or stroke and slept less than 6 hours had three times the increased risk of dying from cancer.
- The increased risk of early death for people with high blood pressure or diabetes was negligible if they slept for more than 6 hours”. [5]
Julio Fernandez-Mendoza, Ph.D., associate professor at Pennsylvania State College of Medicine and sleep psychologist at the Sleep Research & Treatment Center of the Penn State Health Milton S. Hershey Medical Center in Hershey, Pennsylvania was quoted saying, “Our study suggests that achieving normal sleep may be protective for some people with these health conditions and risks.” He went on to say, “Short sleep duration should be included as a useful risk factor to predict the long-term outcomes of people with these health conditions and as a target of primary and specialized clinical practices.”
Hypertension
Even just a single night of poor rest can take its toll on the heart, ramping up pressure in the veins and stretching their delicate walls. A study on young male workers in Japan monitored blood pressure for 24 hours following a night of normal rest and a night of insufficient sleep. They found that heart rate and blood pressure were significantly elevated after missing out on just a few hours of shut-eye.
Another study in China looked at sleep duration and bedtimes in over 37,000 people and discovered that sleeping more than 8 hours and going to bed past midnight were associated with higher rates of hypertension. High blood pressure may seem commonplace in our present day and age, but its insidious effects will steal over 7 million lives this year alone.
Coronary Heart Disease (Coronary Artery Disease)
When the heart becomes damaged from things like smoking, high blood pressure, and a sedentary lifestyle, inflammation occurs and plaque made up of cholesterol, calcium and other waste products begin to build up at the site of injury. This process, known as atherosclerosis, can cause shortness of breath, chest pain (angina), and eventually may lead to a heart attack.
Researchers looked at multiple studies involving 474,684 men and women and found that too little sleep was associated with an increased risk of developing or dying from coronary heart disease. The Nurses’ Health Study that followed 71,716 middle-aged women over a decade also discovered that both short and long sleep durations modestly increased the risk of coronary events, even after controlling for variables like body mass index, smoking, and snoring.
Maybe you’re thinking, “I’m healthy…my heart can handle missing 1-2 hours of shut-eye here and there.” Consider this, another study performed at the University of Chicago tracked coronary artery health and shut-eye in 500 healthy individuals who previously showed no signs of atherosclerosis or heart disease. Researchers discovered that individuals who slept just 5-6 hours a night were 200-300% more likely to develop calcification of the coronary arteries over the next 5 years than those getting 7-8 hours.
Metabolic Diseases
Sleep loss may also increase the risk of developing cardiometabolic diseases, which include obesity, high cholesterol, and type 2 diabetes. Scientists have discovered that sleep restriction induces metabolic changes like inflammation, altered gene expression, and insulin resistance. Together, these altered pathways can lead to weight gain, blood sugar abnormalities, and problems with cholesterol.
You’ve probably heard that a high-fat diet increases cholesterol, which is bad for your heart. But did you know that the amount of rest you get could also impact cholesterol?
Researchers investigated these changes in 2,739 individuals and found that sleeping too little increased inflammation and altered genes that regulate cholesterol. This increases the risk of hypercholesterolemia, which is also the leading cause of atherosclerosis.
Scientists have uncovered a U-shaped relationship between sleep and metabolic changes that can lead to high cholesterol and type 2 diabetes. Compelling evidence from over 20 studies identified a link between sleep duration and type 2 diabetes, with higher reports of the disease in both short and long slumber groups. These studies support the idea of a “sweet spot” for hours of sleep, finding the lowest risk for diabetes in individuals who slept 7-8 h per day. [6][7]
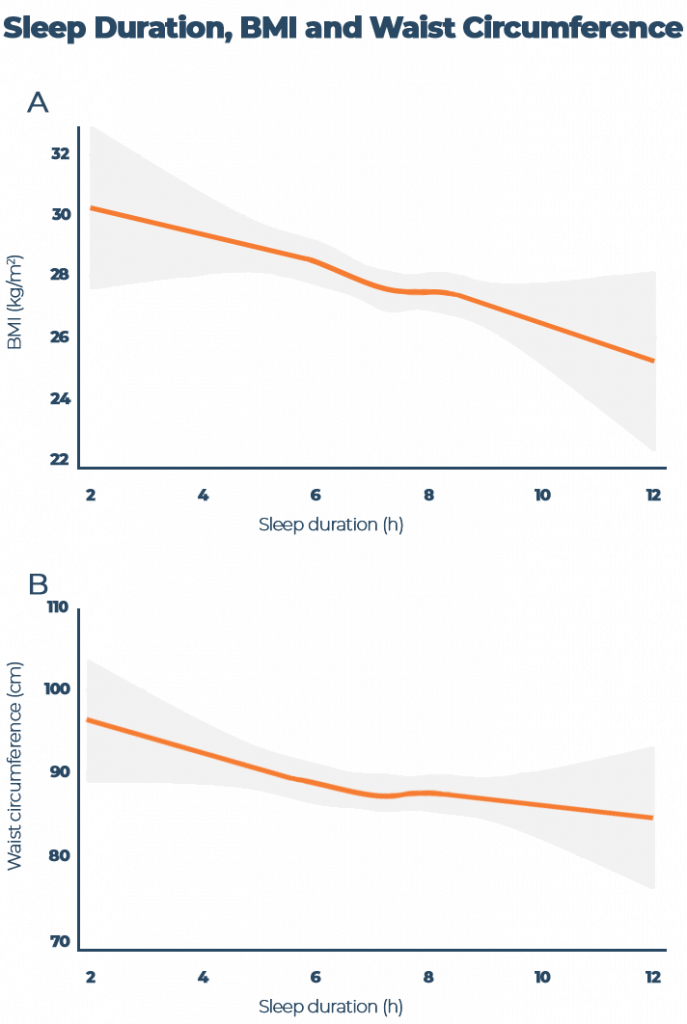
Fast food may not be the only thing to blame when it comes to obesity. A meta-analysis discovered that across 45 studies including 634,511 children and adults from around the world, short sleep duration significantly increased the risk of obesity in both age groups. They also observed a linear relationship between sleep duration and body mass index where-by for every increased hour of rest, body mass index was reduced by 0.35 points.
Another study of UK adults found a similar trend with longer sleep durations associated with lower BMIs and smaller waist circumferences. For every hour of additional shut-eye, both BMI and waist circumference decreased. Now there’s a weight loss tip you’ve probably never heard!
As the obesity epidemic has increased in America and worldwide, so has the weight loss industry, which recently grew to a whopping $72.7 billion annually in the U.S. alone. Unfortunately, most of us give up on our diet and eventually regain all of the weight we lost (and then some) only to start some new fad diet a few months later. According to new research, rather than helping, yo-yo dieting and weight cycling may increase cardiovascular risk factors compared to people who maintain a consistent weight.
Instead of following the latest diet that limits you to eating just a handful of items, it’s better to focus on adopting a healthier lifestyle with the end goal being better health. Along with healthy eating and exercise, sleep therapy may be another step in helping you to achieve your weight loss goals.
Nighttime Disorders Linked To Cardiovascular Health
It turns out that whether your lack of shuteye is due to your own poor sleep habits or you are suffering from a disorder that prevents you from getting the optimal 7-8 hours of rest at night, the deleterious effects on your cardiovascular health are the same. According to the CDC, 70 million American adults suffer from a sleep disorder. A large body of research has identified a link between various sleep disorders and an elevated risk for cardiovascular disease.
Sleep and Cardiovascular Disease
| Underlying Conditions | Elevates Risk For… |
| Obstructive Sleep Apnea | Atherosclerosis Heart Rhythm Abnormalities Congestive Heart Failure Death Metabolic Syndrome Heart Attack Stroke High Blood Pressure Type 2 Diabetes |
| Insomnia | Weight Gain Heart Attack Stroke Death from All Causes |
| Snoring | Early Death after Stroke Trouble Healing after Heart Attack |
Insomnia
Insomnia is the most common sleep disorder in the United States, impacting as many as a quarter of the population. The American Academy of Sleep Medicine defines insomnia as a perceived difficulty with falling asleep, staying asleep, and sleep duration or quality, despite an adequate opportunity for rest. If you suffer from insomnia, you already know that the effects of this disorder extend far beyond the nighttime hours with a significant impact on daytime functioning and overall health.
Over the past decade, multiple studies have associated insomnia with hypertension, coronary artery disease, heart failure, and death as a result of CVD. Scientists believe the underlying mechanisms are likely related to dysregulation of the hypothalamic-pituitary axis within the brain, increased sympathetic nervous system activity, and increased inflammation. One study with just under 5,000 participants found that there was a 29% increase in CVD among those with insomnia or shorter durations of sleep compared to the control group.
For More Information: Best Mattresses for Insomnia
Sleep Apnea
1 in 15 Americans suffer from sleep apnea, a condition that causes affected individuals to periodically stop breathing during the night. Sleep apnea is associated with surges in blood pressure that may cause plaque within the blood vessels to rupture. Other disease factors such as oxidative stress, inflammation, hypoxemia, arousal from sleep, negative intrathoracic pressure, and metabolic factors can also have a negative impact on cardiovascular health.
Cross-sectional results from the Sleep Health Study revealed that among 1,023 participants with sleep apnea, 16% reported one or more manifestations of cardiovascular disease including coronary heart disease, stroke, heart failure, or a combination of these. According to some research, “obstructive sleep apnea increases the risk of heart failure by 140%, the risk of stroke by 60%, and the risk of coronary heart disease by 30%.”
Read More: Best Mattresses for Sleep Apnea
Questions for Your Doctor
Should I be tested for sleep apnea?
Sleep apnea deprives the body and brain of oxygen and places a serious strain on the heart and lungs. Individuals with sleep apnea have significantly increased risks for cardiovascular disorders compared to the general population, but with proper treatment, these numbers drop.
If you frequently snore, wake up with a dry mouth, or feel tired despite getting a full night’s rest, it may be a good idea to speak to your doctor about having a sleep study to rule out sleep apnea. One of the most common treatments is the use of a continuous positive airway pressure machine (CPAP), although other lifestyle changes like losing weight and changing your sleep position may help as well.
How much should I be sleeping per night?
Questioning “Dr. Google” about how many hours of sleep per night is ideal will yield a wide range of results from as few as 5 hours per night to as many as 9-10. Navigating science from fiction can be overwhelming, and it can be hard to know who to trust or what to believe.
Many studies have found 7-8 hours of rest per night leads to the lowest risks for a number of diseases, with anything more or less linked to a worsening of health. In 2017, the American Academy of Sleep Medicine and the Sleep Research Society issued a new joint consensus statement recommending that “adults aged 18 to 60 years should sleep 7 or more hours per night on a regular basis to promote optimal health and reduce the risk of adverse health outcomes.”
While these recommendations are a good starting point, it’s important to remember that every individual is unique, and the right amount of sleep will vary from person to person and even from season to season in life. Speak to your doctor about what is right for you, and consider how you feel after waking, daytime functioning and memory, and overall health to determine if your body is getting the optimal amount of rest that it needs.
Can insomnia be causing my chest pain?
Chest pain can be related to a number of conditions, some serious and others as trivial as some indigestion from the burrito you ate last night. Chest pain that frequently occurs during the night or after a poor night of sleep could be a sign of nocturnal angina, a type of pain or discomfort caused by the heart muscle not getting enough oxygen-rich blood.
Insomnia triggers a stress response within the body, and this could weaken the heart over time. If you suffer from insomnia and are experiencing chest pain or often feel like your heart is racing or skips a beat, speak to your doctor or ask for a referral to a cardiologist for further testing.
What exercise programs are safe for me?
Staying healthy by eating right, sleeping adequate hours, and getting plenty of exercise are some of the most important and often underlooked lifestyle changes that can have a direct impact on heart health. Exercise may also help you sleep better at night – just be sure to exercise earlier in the day or it could have the opposite effect.
If you are new to exercise or have been sedentary for many years, it is important to take it slow and ease back into regular physical activity.
The American Heart Association recommends a good starting goal of 150 minutes of exercise per week, but before you begin you should always speak to your doctor to get the all-clear on whatever form of activity you choose. While staying active is a good thing, for people with certain conditions, some forms of exercise may not be recommended.
Sleep and Healthy Heart

Did you know there is a link between sleep and your heart? Cardiovascular disease is the number one cause of death worldwide, and many of the risk factors are preventable. If you are one of the 1 in 7 individuals who aren’t getting the recommended 7-9 hours of sleep per night, pay attention! Making these small changes could improve your health and might even save your life!
- Find your “sweet spot” when it comes to sleep. 7-9 hours are ideal, but waking feeling alert and energized is the best sign that your body is getting the rest it needs.
- More or less isn’t best. While it may be tempting to skimp on sleep during the week and catch up with a long snooze fest over the weekend, this practice increases stress and weakens the heart.
- Create a sleep routine. Have a consistent bedtime routine and practice going to bed and waking at roughly the same time, 7 days a week. This regulates the sleep-wake cycle and may improve the quality of sleep.
- Optimize your sleep. A dark, cool, and quiet environment with a comfortable, supportive pillow and mattress may improve the quality of your sleep by helping you to fall asleep faster and stay asleep longer.
- Keep the gadgets out. Electronic devices that emit blue light may prevent melatonin release and could harm your sleep. Try to avoid using electronics for at least an hour before bedtime and keep them out of the bedroom.
- Move it and lose it. Exercise and weight loss are not only good for your heart, but they’re good for your sleep as well. Instead of yo-yo dieting which may negatively impact health, focus on eating a healthy diet and avoiding refined sugar.
- Treat sleep disorders. If you are your partner suspect you may suffer from a sleep disorder, it is important to see a doctor. Trouble sleeping, snoring, and excessive drowsiness during the day may be signs that something is wrong.
- Manage stress. Feeling anxious or frequently stressed isn’t healthy. It can take a serious toll on your sleep and your heart. Practice activities that are calming like yoga, deep breathing, and meditation. If needed, seek out a trusted friend or a therapist who can help.
Conclusion
Cardiovascular disease remains the leading cause of death worldwide, killing millions every year. The good news is, it’s preventable! While eating kale and clocking more hours at the gym may not be everyone’s cup of tea, improving your heart health could be as simple as getting the right amount of rest at night.
Maybe one day doctors will prescribe sleep based on its cardioprotective effects, but for now, it’s up to you to take your heart and your health seriously. Try out our 8 healthy heart sleep tips and start catching more zzz’s today!
Sources and References:
[1] Human Heart: Anatomy, Function & Facts, Live Science
[2] Insomnia with Objective Short Sleep Duration and Risk of Incident Cardiovascular Disease and All-cause Mortality: Sleep Heart Health Study, Oxford Academic
[3] Cardiovascular Diseases (CVDs), World Health Organization
[4] Short Sleep Duration and Incident Coronary Artery Calcification, National Center for Biotechnology Information
[5] Sleeping Less than Six Hours and Heart Disease, Stroke – Deadly Combo, Newsroom
[6] Quantity and Quality of Sleep and Incidence of Type 2 Diabetes, Diabetes Journals
[7] Sleep Duration and Risk of Type 2 Diabetes: A Meta-analysis of Prospective Studies, Diabetes Journals

Raina Cordell
RN, RHN, Certified Health Coach
About Author
Raina Cordell is a Registered Nurse, Registered Holistic Nutritionist, and Certified Health Coach, but her true passion in life is helping others live well through her website, www.holfamily.com. Her holistic approach focuses on the whole person, honing the physical body and spiritual and emotional well-being.
Combination Sleeper
