Melatonin has grown in popularity in recent years as a natural sleep aid. For adults, it has shown to be a safe, non-habit-forming alternative to prescription sleeping pills.
Like adults, kids can have difficulty sleeping. This raises the question, then, as to whether melatonin is helpful for children. In this article, we’ll go over common reasons kids of various ages have issues sleeping in the first place, when melatonin might be helpful (or harmful), the appropriate dosage, and alternative supplements and habits that should help your kids – and you – get good sleep.
Sleep Problems in Kids
Similar to adults, kids can have problems sleeping for a variety of reasons, from stress and anxiety to underlying medical conditions. Additionally, sleep problems can be both temporary and long-term. Below are some of the most common reasons behind childhood insomnia1.
- Another sleep disorder (like restless leg syndrome or sleep apnea)
- Anxiety or stress (this could be situational stress, or prolonged, like an anxiety disorder)
- A medical, mental, or developmental condition (for example, asthma, an illness, depression, anxiety, ADHD, autism)
- Certain medications (like antidepressants, steroids, or stimulant medications2 for ADHD
- Caffeine
- Unhealthy food habits3 (including skipping breakfast, eating fast food, and regularly eating sweets)
- Increased screen time
- Being overweight/obese
What Parents Should Know About Melatonin
Melatonin4 is a hormone that each of our bodies naturally produces in a small, pea-sized gland in the brain called the pineal gland. The job of this gland is to receive information from the eyes about the world around you – and answer the question, is it dark or light outside?
If it is dark out, the pineal gland will begin producing melatonin. This usually happens about two hours before going to sleep. On the other hand, if it is still light outside or if you are looking at bright lights (including screens), melatonin synthesis becomes inhibited5, and the body’s circadian rhythm for melatonin will be thrown off because the light resets it.
This is why screen time is listed as one of the most common reasons behind childhood insomnia.
Melatonin supplements can be used to give the body a boost in its melatonin production. These types of supplements are typically made synthetically and can be taken in a variety of forms including gummies, pills, liquids, or powders. Most experts have deemed short-term use of melatonin6 supplements to be safe, however, there are some things to keep in mind for children in particular.
Melatonin has another, lesser-known function, and that is its vital role in puberty. According to a 2019 study7, melatonin is produced in larger quantities in children before puberty. Sometime between the ages of 8 and 13 (on average) in females and 9 and 14 in males, the body’s natural production of melatonin drops sharply, which is believed to play a role in triggering the onset of puberty.
What, then, does adding a melatonin supplement do to children whose melatonin is supposed to be dropping in order to go through puberty? What does adding supplemental melatonin do to children who haven’t gone through puberty, and who naturally produce larger quantities of melatonin?
Most importantly, is this safe?
Is Melatonin Safe for Kids?
As we mentioned, melatonin is naturally produced in younger children in larger quantities. More specifically, it looks like this8: Children between 18 months and six years of age have the highest amount of melatonin, then there is a slight drop off between ages 6-8, followed by a drastic drop off between ages 8-13. Once puberty is triggered after this dropoff, it rises slightly again but never again to the levels pre-puberty8. The level gradually decreases9 thereafter throughout our lives.
Nightmares
When melatonin levels are high, studies10 show that we spend more time in Rapid Eye Movement (REM) sleep. REM is the sleep stage when our brain activity increases, and we are more likely to have vivid or intense dreams or even nightmares.
This is why children, who naturally produce more melatonin than adults, often spend more time in REM sleep11 and can have wilder dreams and more nightmares. Additionally, it’s why one of the most common side effects of melatonin supplements, especially in children under 8, is nightmares.
Now, this doesn’t necessarily mean that melatonin is unsafe for children. If your child is having nightmares due to melatonin supplements, you could consider lowering the dosage (which we’ll discuss in the next section) or stopping the supplements entirely.
As always, do not add a supplement or change a dose of supplements for kids unless speaking with their pediatrician.
Puberty
There is some concern, though, that supplementing with melatonin around the age of puberty (typically sometime between 8-14) could delay its onset.7 Studies in the area are limited, but if you want to be cautious, you can avoid giving your kids melatonin supplements before the onset of puberty. After all, the body goes through an important natural transition between a very high amount of melatonin and a drastic drop during this period of life.
Once puberty has begun, though, short-term, low-dose melatonin could be safe for most adolescents and teenagers.
More Serious Effects
Short-term and low-dose melatonin appears to be safe for children of most ages, with the most common side effects12 being nightmares, grogginess, headaches, or dizziness, all of which go away upon discontinuation, and the possible side effect of delaying the onset of puberty. However, there are some more serious side effects reported when children either intentionally or unintentionally consume too much melatonin.
According to the Centers for Disease Control and Prevention (CDC)13, between the years 2012-2021, the number of melatonin-related calls to poison control went up by 530 percent. Most of these calls were regarding children under five who had accidentally ingested too much melatonin. Kids’ melatonin is often sold as gummies; they taste good and could be eaten like candy for those who don’t understand.
Most, but not all, of these ingestions (by ingestions, the CDC means substances ingested and reported to poison control) were harmless. In this CDC study, about 80 percent of children had no symptoms. Of those who reported side effects, the main symptoms were drowsiness, upset stomachs, vomiting, and headaches. During this 10-year period and out of more than 260,000 ingestions, about 4,000 children were hospitalized, a handful of whom were put on ventilators. Most of the hospitalized children were teenagers who had intentionally attempted to overdose on melatonin.13
Melatonin Dosage for Kids
You should discuss dosing with your child’s primary care provider before starting or changing any melatonin dosage. Here, we will share some general information based on research, but we want to emphasize that talking with your child’s healthcare provider is an important first step.
The consensus seems to be that because children naturally produce higher levels of melatonin and their melatonin levels fluctuate in order to go through puberty, if you do decide to supplement with melatonin, it should be at the lowest possible effective dose, for a short period (less than three months).
You can start with a dose as low as 0.5-1 milligram14 (the lowest possible effective dose). If this isn’t effective, you can increase the dose up to the maximum recommended dose. This maximum recommended dose will depend on their age and what your child’s doctor also suggests.
Under 3 Years Old
According to Boston Children’s Hospital, children under three should not use melatonin at any dose. Children at this age are producing enough melatonin on their own and difficulties falling and staying asleep are almost always behavioral in nature.12
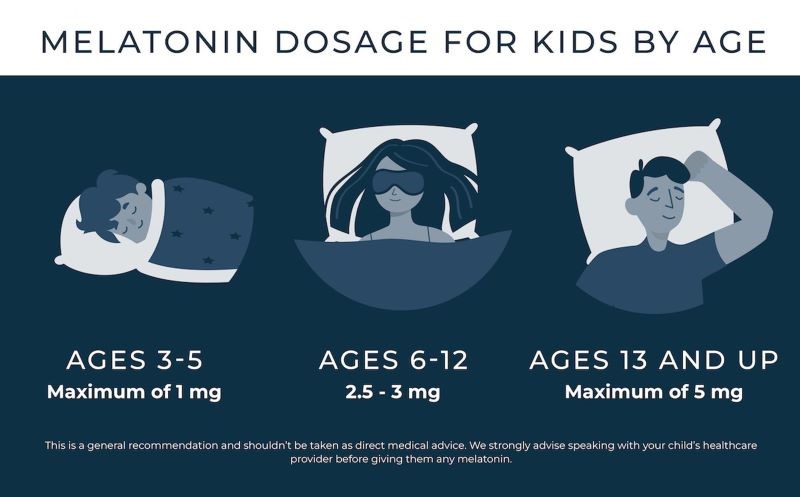
3-5
Physicians recommend 1 milligram or less15 of melatonin in children 3-5 years of age.
6-12
Physicians recommend a maximum of 2.5-3 milligrams of melatonin in children between ages 6 and 12.15
Note: There is some evidence that using melatonin around the onset of puberty could cause a delay in onset, though more information is needed.7
13 and Up
Physicians recommend a maximum dose of 5 milligrams of melatonin for those 13 and up.15
Melatonin and Neurodevelopmental Disorders
Children with neurodevelopmental disorders are more likely to have trouble sleeping than other children. Autism Spectrum Disorders (ASDs), in particular, are associated with trouble sleeping. In fact, over 50 percent16 of children with ASDs report trouble sleeping.
There is some evidence that melatonin regulation might be abnormal in children with autism, and studies show that supplementing with melatonin for kids on the spectrum is helpful for sleep.16
Additionally, a study in 201817 found that children with a variety of neuromedical disorders (including ADD, ADHD, Autism Spectrum Disorder, motor disorders, specific learning disorders, and communication disorders) all benefited from a daily 4-milligram melatonin supplement. They found an improvement in all of the following areas: temperament upon waking, sleepiness after waking up, stereotypical behavior, irritability, hyperactivity, and inappropriate speech.17
Their conclusion, and the conclusion of many researchers in recent years, is that long-term melatonin supplementation seems to be safe and particularly helpful for some children with neuromedical disorders. Of course, research on the subject is still relatively new, and more needs to be done though it does seem promising.
Doctors recommend a maximum dose of 10 milligrams of melatonin for children with neuromedical disorders.15
For any children who aren’t having trouble sleeping and you’d just like to help them get “better” or more “restful” sleep, doctors advise against melatonin.13
Melatonin Alternatives
If you’re struggling to get your kids to sleep, melatonin supplements might help, but even so, they are only a temporary fix (recommended for a max of three months for most children).
You may even be tempted to go for something stronger, like a prescription medication. In fact, prescription medications are often the first line of defense for insomnia in both children and adults. Studies18 point out, though, that this is troubling because there are no FDA-approved medications for the treatment of insomnia in children, and there are concerns about the safety and side effects of the off-label medications doctors prescribe. Plus, evidence19 indicates that while pharmacological treatments may have rapid short-term effects on sleep problems, they typically don’t have long-term positive effects on sleep.
The key is going to be doing the hard work of fixing the underlying issues or behaviors leading to sleeplessness in the first place.
Cognitive Behavioral Therapy for Insomnia20 (or CBT-i) is one alternative to melatonin or sleep aids that shows real, long-lasting results for people of all ages. This treatment involves behavioral changes, such as bedtime shifts (including something called “sleep restriction”), stimulus control, thought challenging, psychoeducation, and various relaxation techniques.20
A 2015 meta-analysis21 found that CBT-i was as effective as sleep medication, with zero side effects, fewer episodes of relapse, and a tendency for sleep to continue to improve long past the end of treatment. The research concluded that CBT-i is the most effective non-pharmacological treatment for insomnia.21
Read More: Magnesium vs Melatonin – Which Aid Is Better for Sleep?
Tips to Improve Kids’ Sleep
Whether you and your kids choose to supplement with melatonin or not, the most important changes you can make are behavioral and environmental; in other words, practicing good sleep hygiene.
Experts recommend that children who can’t sleep:
- Avoid napping during the day (for children over preschool age)
- Have dinner at least two hours before bedtime
- Stop using screens at least one hour before bedtime
- Establish a regular and consistent bedtime routine: going to bed and waking up at the same time every day (even for older kids)
- Reading before bed (or if they are young, you can read to them)
- Sleep in their own beds
- The sleep environment should be dark and quiet
- The room should be cool
Additionally, The Society of Behavioral Medicine22 advises that the bed be used for sleep only. Using the bed for playtime or homework can confuse the brain, associating the bed with more than sleep. If an older child is having trouble sleeping, encourage them to get up out of bed and do something quiet until they are sleepy again, and then go back to bed.
Daily exercise is also important for kids of all ages when it comes to general physical and mental health, including getting good sleep.22
If you’re wondering how much sleep your child should be getting according to their age, The American Academy of Sleep Medicine23 recommends the following:
- 4 to 12 months – 12 to 16 hours
- 1 to 2 years – 11 to 14 hours
- 3 to 5 years – 10 to 13 hours
- 6 to 12 years – 9 to 12 hours
- 13 to 18 years – 8 to 10 hours
Conclusion
Children of all ages can struggle to get to sleep or stay asleep at various times, and it can be tempting to reach for a quick fix like medication. Unfortunately, there’s no magic pill that will help your kid with sleep, and in fact, prescription sleep aids come with a slew of side effects and haven’t been approved by the FDA for children.
Melatonin seems to be a relatively safe short-term, natural sleep aid for kids when used at a very low dose. However, it does come with some risks, and the long-term effects on things like puberty are not yet known. The only real way to improve sleep long-term is to resolve the root of the problem with something like CBT-i, or at the very least, practicing good sleep habits.

Natalie Grigson
Writer
About Author
Natalie is a content writer for Sleep Advisor with a deep passion for all things health and a fascination with the mysterious activity that is sleep. Outside of writing about sleep, she is a bestselling author, improviser, and creative writing teacher based out of Austin.
Combination Sleeper
References:
- “Insomnia”. Boston Children’s Hospital. Webpage accessed December 15, 2023.
- Stein, Mark A., Weiss, Margaret., Hlavaty, Laura. “ADHD treatments, sleep, and sleep problems: complex associations”. Neurotherapeutics. 2012.
- “Insufficient sleep in children is associated with poor diet, obesity and more screen time”. American Academy of Sleep Medicine. 2018.
- Arendt, J., Aulinas, A. “Physiology of the Pineal Gland and Melatonin”. Endotext. Last modified October 30, 2023.
- Gooley, Joshua J., et al. “Exposure to Room Light before Bedtime Suppresses Melatonin Onset and Shortens Melatonin Duration in Humans”. The Journal of Clinical Endocrinology and Metabolism. 2011.
- Bauer MD, Brent A. “Is melatonin a helpful sleep aid — and what should I know about melatonin side effects?”. Mayo Clinic. Last modified October 28, 2023.
- Boafo, Addo., et al. “Could long-term administration of melatonin to prepubertal children affect timing of puberty? A clinician’s perspective”. Nature and Science of Sleep. 2019.
- Molina Carballo, A., et al. “Pineal functioning (melatonin levels) in healthy children of different ages. An update and the value of pineal gland study in pediatrics”. National Library of Medicine. 1996.
- Karasek, M. “Melatonin, human aging, and age-related diseases”. National Library of Medicine. 2004.
- Kunz, Dieter., et al. “Melatonin in patients with reduced REM sleep duration: two randomized controlled trials”. National Library of Medicine. 2002.
- “Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem”. National Library of Medicine. 2006.
- Fliesler, Nancy. “Melatonin for kids: Is it effective? Is it safe?”. Boston Children’s Hospital. 2023.
- Lelak MD, Karima., t al. “Pediatric Melatonin Ingestions — United States, 2012–2021”. Centers for Disease Control and Prevention. 2023.
- Esparham MD, Anna. “Melatonin for Kids: What Parents Should Know About This Sleep Aid”. Healthy Children. Last modified September 26, 2023.
- Janjua MD, Irvin., Goldman MD, Ran D. “Sleep-related melatonin use in healthy children”. Canadian Family Physician. 2016.
- Devnani, Preeti A., Hegde, Anaita U. “Autism and sleep disorders”. Journal of Pediatric Neurosciences. 2015.
- Yuge, Kotaro., et al. “Long-term melatonin treatment for the sleep problems and aberrant behaviors of children with neurodevelopmental disorders”. BMC Psychiatry. 2020.
- Vriend, Jennifer., Corkum, Penny. “Clinical management of behavioral insomnia of childhood”. Psychology Research and Behavior Management. 2011.
- Ramchandani, P., Wiggs, L., Webb, V., Stores, G. “A systematic review of treatments for settling problems and night waking in young children”. BMJ. 2000.
- Dewald-Kaufmann, Julia., de Bruin, Ed., Michael, Gradisar. “Cognitive Behavioral Therapy for Insomnia in School-Aged Children and Adolescents”. National Library of Medicine. 2023.
- Rossman PhD, Jeffrey. “Cognitive-Behavioral Therapy for Insomnia: An Effective and Underutilized Treatment for Insomnia”. American Journal of Lifestyle Medicine. 2019.
- Stager, Lindsay M., Caldwell PhD, Angela., Bates PhD, Carolyn., Laroche MD, Helena. “Helping Kids Get the Sleep They Need”. Society of Behavioral Medicine. Webpage accessed December 15, 2023.
- “Importance of good sleep routines for children”. The University of British Columbia. 2018.